Infancy and early childhood are a time of great growth and new accomplishments--more than at any other time in a person’s life. But children continue to develop and acquire new skills as they age. Let’s discuss some of the activities and skills a preschool child should be mastering. Preschool refers to the ages of 3 to 5 years old.
A preschooler should already be able to get to standing, walk, and run, but they will be refining these skills by getting faster, smoother, more coordinated and more controlled. As they age, their attention span should increase and their verbal skills improve. They will be able to jump forward for longer distances, start at to hop on 1 foot, and enjoy more active play.
At this age children are starting to engage in play with others, imitate movements, and have more goal-directed behaviors. They are easier to guide in play and can communicate with improving clarity and content. They are learning basic skills that they will need to start kindergarten.
A Basic List of Preschool Skills Include:
GROSS MOTOR SKILLS
3-4 years:
Locomotor Skills: jump forward 26 inches, runs pumping arms and pushing off balls of feet with a forward lean of the trunk, able to run and make sharp turns, gallops
Balance Skills: walks forward on a line for 4 feet without stepping off line. Walks backward 4 feet without stepping off line
Tricycle Skills: pedals and steers a tricycle
Ball Skills: throw a tennis ball underhand at a target 5 feet away, throws a tennis ball overhand to a target 5 feet away, catches a large ball with hands, elbows bent, able to kick a stationary playground ball
5 years:
Locomotor skills: hops forward on either foot for 5 hops, skips 10 feet with good rhythm
Ball Skills: catches a tennis ball with 2 hands from a distance of 5 feet, kick a moving playground ball
Balance Skills: stands on tip toes for at least 8 seconds, stands on 1 foot for 10 seconds, able to perform 3 sit ups
FINE MOTOR SKILLS
- Button and unbutton large buttons
- Paste things onto paper
- Use crayons to color and draw while holding the writing instrument with thumb and fingers
- Uses non-dominant hand to steady writing surface
- Build a tower of 10 blocks
- Complete puzzles of 5 or more pieces
- Zip and unzip a zipper
- Imitate or copy a cross or circle
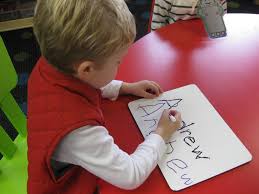
- Trace letters and begin writing their name
LANGUAGE SKILLS
- Names colors
- Names basic shapes
- Able to count to 10 alone and higher with help
- Is clearly understood when speaking
- Understands categories like animals, food, toys, clothes
COGNITIVE SKILLS
- Can remember a sequence of events with 2-3 steps
- Matches shapes and colors


- Knows some letter names
- Sorts objects into groups
- Enjoys imaginative play like playing house
- Understands concepts like “one” and “many”
- Makes comparisons
SELF HELP SKILLS
- wash hands
- brush teeth

- Comb hair
- put on and remove clothes
- put shoes on the correct feet
- use a fork and knife
Support for Your Child
Exposing your child to different activities and encouraging curiosity and exploration are wonderful ways to help your child develop these skills. Playing basic board games and puzzles like Candyland, Memory Caps, or Chutes and Ladders teach turn taking, numbers, sequences, and memory.
Some older preschoolers may enjoy participating in a sport such as Little League or soccer. Many YMCAs or community centers have basic swim classes or gymnastics geared toward little ones. Enrolling in several short-duration classes can expose your child to lots of new movement patterns and experiences and lets them decide what type of sport they might like to pursue later.
Most community libraries have great programs including reading and listening skills, crafts, and special events. These are a fabulous way to let your child participate with peers and gain new skills.
If your child has not accomplished the majority of the above skills by five years old or the start of kindergarten, you may want to consider a screening or evaluation by a Physical Therapist, Occupational Therapist or Speech and Language Pathologist (Speech Therapist). Talk with your pediatrician and access local resources for evaluation clinics or programs.
Blog Administrator: Trisha Roberts
proeducationaltoys@gmail.com
Copyright © 2017 TNT Inspired Enterprise, LLC, All rights reserved.
Unauthorized duplication is a violation of applicable laws.